Labor in the Hallway, Delivery in the ED: A Regional Hospital Under Scrutiny
Case #23 ER Overcrowding, Missed Escalation, and a Regional Hospital’s Defense
On a spring morning in 2022, Jane (a pseudonym for confidentiality) entered the emergency room at RV Regional Hospital (a pseudonym for privacy), 22 weeks into her pregnancy. She was bleeding and in pain. For more than three hours, she labored in a crowded ER hallway, unmonitored and without meaningful assistance. By the end of that day, she would deliver her son alone in an unsterile ER room, holding onto the chair handles as contractions overcame her. Her baby fell onto the chair, hitting his head on the armrest, while a nurse, according to the complaint, stood in disbelief.
Two years later, her lawsuit against the hospital, physicians, and their insurers would bring forward dueling narratives from expert witnesses on both sides, raising complex questions about standard of care, viability, documentation failures, and the psychological toll of traumatic birth experiences.
OB/GYN Access and ER Overcrowding in Regional U.S. Hospitals
This case highlights systemic challenges common in regional hospitals across the United States. Many of these facilities serve as referral centers for surrounding rural areas, but often face:
Limited or inconsistent on-site OB/GYN coverage: Leaving ER physicians to manage obstetric emergencies without immediate specialist support.
No or limited NICU capabilities: Premature neonates often cannot receive advanced care locally, requiring transfer.
Overcrowded emergency departments: With staff stretched thin, ER teams must triage critical patients while managing obstetric complications.
Across the U.S., regional hospitals operate with constrained resources and must balance stabilizing patients with arranging timely transfers to tertiary centers. ER physicians in these settings often rely on outdated protocols or lack access to rapid tele-OB consultation. These systemic gaps, even in high-resource countries, can lead to similar outcomes if hospitals do not invest in multidisciplinary response systems.
The Allegations
In her second amended complaint, Jane alleged that Dr. JC, the ER physician, and the hospital staff:
Delayed performing a pelvic exam despite her worsening symptoms.
Failed to consult obstetric specialists in a timely manner.
Left her unmonitored in a corridor for hours while she bled and experienced severe pain.
Neglected to prepare for imminent delivery or provide her with adequate analgesia or emotional support.
The lawsuit also claimed that hospital nurses dismissed her pleas for help, allegedly mistaking active labor for blood clots. Jane's baby, John, was born alive but died within 35 minutes of delivery. The plaintiff argued that earlier intervention could have prolonged the pregnancy or changed the outcome.
The Plaintiff’s Experts: A Story of Neglect and Missed Opportunities
Dr. M (Obstetrician)
Dr. M’s report described critical failures in triage, monitoring, and escalation of care. He observed that the patient’s placement in a hallway for over three hours, despite signs of active labor and vaginal bleeding, represented a serious lapse in standard obstetric practice. According to his analysis, this delay eliminated any window of opportunity for meaningful intervention.
M further highlighted the absence of a multidisciplinary response, noting that a rapid response team—including obstetric, neonatal, and anesthesia services—should have been mobilized immediately. He also addressed the emotional harm of being left in a hallway, stressing how psychological trauma compounded the physical risks.
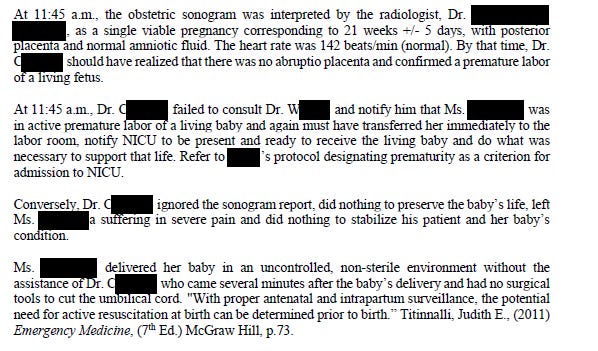
He also detailed specific moments where he believed the ER team missed critical opportunities to intervene and failed to act on diagnostic findings:
Dr. G (Obstetrician)
G underscored the ethical considerations in extreme prematurity cases. He noted that in many jurisdictions, families are offered resuscitation options at 22 weeks gestation, but no such discussion occurred here. This omission, he argued, deprived the patient of informed consent.
G also conducted a detailed analysis of the medical record, highlighting inconsistencies between recorded observations and likely real-time events. He noted that several progress notes were entered hours after the events they described and identified discrepancies between staff testimony and patient accounts. According to G, these issues undermined confidence in the medical record and made it more difficult to assess the quality of care provided.
This excerpt from Dr. G’s report shows how he dissected the chart entries and timeline to highlight potential documentation failures:

This focus on documentation integrity reinforced the plaintiff’s broader argument that systemic and individual failures converged to create a preventable outcome.
Dr. R (Psychologist)
R provided an assessment of the patient’s psychological trauma, linking her PTSD symptoms to the experience of delivering alone and unsupported. She described how repeated invalidation from staff likely exacerbated feelings of helplessness and betrayal—hallmark features of birth trauma.
Dr. R outlined specific psychological and socioeconomic damages she attributed to the traumatic delivery and loss, as well as recommendations for intensive mental health care:

R projected that the patient’s recovery would require years of therapy and support.
The Defense Experts: Previability and Standard Care
Dr. AV (Obstetrician & Sonography Specialist)
AV focused on fetal metrics and maternal safety. He argued that given the estimated gestational age of 21 weeks and evidence of chorioamnionitis, any aggressive intervention would have posed unacceptable risks to maternal health without improving the neonatal prognosis. He also discussed resource limitations typical in regional hospitals.
In defending the ER team’s choice to prioritize a sonogram before performing a pelvic exam, AV noted that the patient did not bring her prenatal chart to the hospital. This, he argued, prevented the ER team from confirming gestational age or ruling out placenta previa without imaging. While this point bolsters his rationale for performing a sonogram first, it stands out as contextually unusual in U.S. healthcare systems, where electronic records or direct communication with a patient’s OB would typically fill such gaps. This framing may also reflect a subtle rhetorical move to shift part of the responsibility to the patient, deflecting from the ER team’s obligation to obtain critical history through other means.
In his report, AV explains why the lack of prenatal records necessitated a sonographic evaluation before proceeding to a pelvic exam:

AV also addressed the plaintiff’s contention that interventions like antenatal steroids or tocolytics might have prolonged the pregnancy. He argued that these treatments were contraindicated due to the presence of intrauterine infection, and that observation alone was the only medically sound option:

Dr. MC (Emergency Medicine)
MC defended the ER team’s approach, stating that the patient’s initial presentation did not warrant an emergent OB consult. He maintained that observation and periodic reassessment were reasonable under the circumstances. MC acknowledged ER overcrowding as a contributing factor but asserted that the team acted within standard practice.
This excerpt from the ER documentation captures the sequence of events leading up to the sonogram:

The obstetric sonogram findings became a central piece of evidence, with both plaintiff and defense experts interpreting the data to support their narratives.

Dr. C (Neonatology)
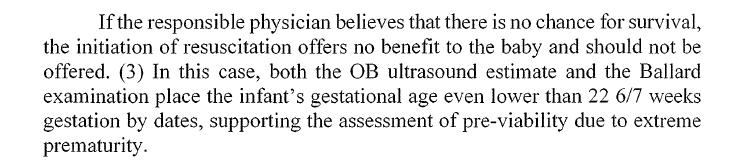
C addressed the futility of neonatal resuscitation at 21–22 weeks, stating that survival rates are exceedingly low and comfort care was the only medically sound option. She also highlighted the NICU’s adherence to established national guidelines for cases of extreme prematurity. This excerpt from Dr. C’s report captures her rationale for deeming resuscitation inappropriate, a point that would later draw sharp disagreement from the plaintiff’s experts:
She further documented the baby’s condition and the clinical decisions made in the minutes after delivery:

Legal Strategy and Resolution
The litigation in this case involved several strategic maneuvers and procedural complexities that attorneys on both sides had to navigate:
Motions in Limine Battles: The plaintiff moved to strike defense motions that violated a prior court order requiring a single omnibus filing. These disputes highlight the importance of strict compliance with procedural orders and how violations can shift judicial favor.
Cross-Claims and Indemnity Disputes: Midstate Emergency Group (a pseudonym) filed cross-claims arguing that RV Regional Hospital (a pseudonym) was contractually obligated to indemnify them for any liability. This created additional layers of litigation, requiring attorneys to manage both the primary malpractice allegations and secondary contractual disputes.
Expert Witness Strategy: Both sides leaned heavily on expert testimony to establish or rebut claims of negligence, viability, and emotional harm. Strategically timing disclosures and challenging opposing experts on methodology were key components of pretrial maneuvering.
Confidential Settlement: In July 2025, the court entered judgment dismissing the case with prejudice following a confidential settlement agreement between the plaintiff and RV Regional Hospital. While the settlement amount remains undisclosed, the court retained jurisdiction to enforce the terms of the agreement, indicating the parties negotiated enforceable obligations post-dismissal.
This phase of the case highlights how procedural tactics, indemnity issues, and settlement negotiations can significantly influence the outcome before a jury hears the evidence.
Lessons for Attorneys and Expert Witnesses
Document Credibility Matters: Plaintiff experts flagged charting inconsistencies, such as progress notes that appeared to have been entered after the fact and discrepancies between the recorded physical exams and the patient’s recollection of her care. These concerns raised questions about the reliability of the medical record and provided fertile ground for cross-examination.
Viability and Maternal Risk: The case illustrated how expert testimony can sharply diverge on issues of fetal viability at 22 weeks. Plaintiff experts highlighted emerging literature supporting resuscitation in micro-preemies, while defense experts emphasized maternal risks, chorioamnionitis, and the low likelihood of neonatal survival. Attorneys must be prepared to navigate these nuances when building their case.
Psychological Trauma Adds Damages: The psychologist’s report highlighted the long-term psychological consequences of unsupported and traumatic childbirth. Attorneys on both sides should recognize that emotional harm, particularly PTSD, can substantially increase the value of damages and shape jury perceptions.
Systemic Failures as a Legal Theme: Beyond individual clinician errors, the plaintiff framed the case as a systemic failure, pointing to ER overcrowding, absence of multidisciplinary protocols, and lack of escalation pathways. For attorneys, identifying and developing these themes can strengthen claims of institutional negligence.
This case highlights the complexity and emotionally charged nature of ER presentations that can evolve into high-stakes litigation, particularly in regional healthcare settings with limited resources.
Key Takeaway for Experts: Comprehensive, defensible reporting that bridges clinical findings with ethical and legal considerations often shapes which narrative dominates in court.
Need Expert Medical or Scientific Research for Your Case?
Contact me at librarian@grahammedlegalresearch.com to ensure your next case is built on solid research.
Website: Graham MedLegal Research, LLC.




